When I was studying public health, my professors would invariably get around to pointing out to the physicians in the class that running water and window screens had saved more lives than physicians ever would. In the ensuing 35 years the balance of payments has moved rather dramatically in the favor of curative medicine when compared to the payments needed to maintain the health of the population. As we come out of a (hopefully) once in a lifetime pandemic, the nation’s health infrastructure is about to get a huge boost from the $1.9 trillion Coronavirus relief package with the money to be spent over one to two years. By comparison, the Affordable Care Act was slated to cost a little under $1 trillion over 10 years. Although much of the funding is framed as Covid -19 specific, as we have found out activities spent to prevent Covid-19 also work to prevent other things such as influenza. The spending that can be identified as health related is categorized as either public health, improved access via health insurance affordability, or funding targeted to improve the “social determinants” such as food, housing, and income security.
Funding for public health focused activities totals almost $93 billion. The main public health provisions are as follows:
- The Centers for Disease Control gets $10.75 billion. This money goes for COVID–19 vaccine distribution and administration and supported activities include the establishment and expansion of community vaccination centers and mobile vaccination units, particularly in underserved areas. It also supports transportation of individuals to vaccination, particularly underserved populations. These is also money to promote vaccine confidence, information, and education activities. On the science side there is money for SARS-CoV-2 genomic sequencing and surveillance as well as data modernization and forecasting.
- The Food and Drug Administration gets $500 million for activities around COVID-19 vaccine safety.
- For public health manpower needs there is $55.56 billion. This money is for testing, contact tracing, surveillance, and mitigation activities including increasing contact tracing capabilities. In addition, there is money for State, local, and territorial public health departments to hire and train case investigators, contact tracers, social support specialists, community health workers, public health nurses, disease intervention specialists, epidemiologists, program managers, laboratory personnel, informaticians, communication and policy experts, and any other positions as may be required to prevent, prepare for, and respond to COVID–19. There is some additional money for the medical reserve corps.
- The community health centers get $7.6 billion for activities including COVID-19 vaccine distribution and administration, testing, contact tracing, mitigation, workforce enhancement, and community outreach and education.
- There is $16.05 billion to support the supply chain for COVID-19 vaccines from development to distribution and to enhance use of the Defense Production Act for the purchase, production, or distribution of medical supplies and equipment for COVID-19.
- The Indian Health Service gets $2.34 billionfor COVID-19 vaccine distribution and administration ($600 million); testing, contact tracing and mitigation ($1.5 billion); and public health workforce for COVID-19 ($240 million).
Funding for individual health coverage included in the bill focuses on making health insurance more affordable but not on systemic change
- Many people who found “Obamacare policies” unaffordable will now be able to purchase insurance through the ACA premium tax credit expansion. This provision lowers the monthly premium for those who purchase coverage through the exchange and in particular for those who are just above the previous coverage “cliff.” During 2021 and 2022, individuals and families above the income cutoff can access premium tax credits. They will also pay no more than 8.5 percent of their household income for a plan purchased through the state or federal marketplaces. Nearly 15 million uninsured Americans could now qualify for subsidies if they enroll through the federal or state marketplace, the Department of Health & Human Services estimates.
- Those who lose their jobs will be able to continue on their current insurance because of COBRA subsidies included in the bill. 100% of the cost of insurance premium will be subsidized for those who lose their jobs for up to 36 months
- Those who need help and support the most will (hopefully) be able to get it through expanded Medicaid benefits and coverage. The improved benefits include increasing funding to states for home- and community-based services, allowing states to offer 12 months of postpartum coverage for new mothers, requiring the coverage of COVID-19 vaccines and treatment for Medicaid enrollees, and expanding COVID-19 testing for people who are uninsured. In addition, reducing disparities will be a priority. There are also new incentives for the 12 “hold-out” states (of which Alabama is one) that have not yet expanded their Medicaid program under the ACA. This expansion would extend Medicaid benefits in those states to households with incomes up to 138 percent of the federal poverty level, an evidence based approach to improving the health and wellbeing of a state’s low-income population.
Lastly, there is funding to support those Americans who are on the lower end of the economic spectrum. Many believe this to be the most significant piece of anti-poverty legislation passed since the Social Security was initiated during the New Deal.
- Support for all Americans will come through extensive poverty abatement funding. There are direct payments of $1,400 to most Americans in addition to the $600 in aid provided in the December stimulus bill. The legislation also extends emergency unemployment benefits beyond their March expiration date to September 6 and increases the child tax credit. Under current law, most taxpayers could claim up to $2,000 per child. In a significant change, the bill would increase the tax break to $3,000 for every child age 6 to 17 and $3,600 for every child under the age of 6. It also provides $20 billion in rental assistance plus $510 million for the FEMA Emergency Food and Shelter Program to support organizations that provide services to homeless people.
- Support for housing security with about $27 billion going towards emergency rental assistance. This is targeted towards low-income individuals. Household income cannot exceed 80 percent of the area median income, at least one household member must be at risk of homelessness or housing instability, and individuals have to qualify for unemployment benefits or have experienced financial hardship (directly or indirectly) because of the pandemic.
- Support for food security. About 10% of Americans, or 22.5 million people, reported they sometimes or often do not have enough to eat on a weekly basis. There is $1.15 billion in targeted funding to continue an increase in the maximum Supplemental Nutrition Assistance Program through September 2021. In addition, money is included to provide food security for low-income mothers and their children, the elderly, and residents of Puerto Rico, Samoa, and the Northern Mariana Islands.
- Support for younger Americans who are entering an uncertain workforce will come through Americorps. The legislation includes nearly $1 billion in funding over three years for AmeriCorps to expand national-service programs to respond to the pandemic. This is a 100% increase. AmeriCorps budgets in recent years have hovered around $1 billion a year. The funding will be primarily directed to existing programs to increase the living allowances paid to AmeriCorps members and expand their ranks, though AmeriCorps officials are still sorting out the details.
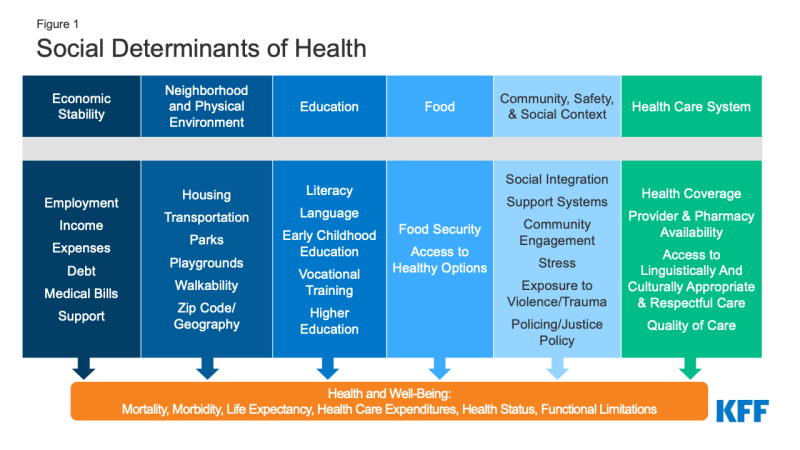
In summary, this bill supports enhanced care access, strengthens the public health infrastructure, and directly attacks poverty, one of the root causes of poor health. It will take the efforts of all of us to make sure that these resources are put to good use.

Leave a comment
Comments feed for this article